What is the Pancreas?
The pancreas is a gland that lies behind the stomach. It plays a major role in the digestion of food as it produces and releases insulin into the bloodstream to regulate blood sugar levels and also secretes digestive enzymes into the small intestine to absorb the remaining food that has passed through the stomach.
What is Chronic Pancreatitis?
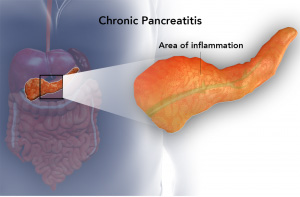
When the digestive enzymes produced by the organ get activated while still in the pancreas, they can cause inflammation of the pancreas and lead to a condition called pancreatitis. It can be further classified as either chronic or acute pancreatitis.
Chronic pancreatitis is persistent pancreatitis that does not heal and leads to progressive deterioration of the pancreas.
When a tumor or gallstone blocks the pancreatic duct, it results in the accumulation of pancreatic enzymes within the pancreas. Consequently, these enzymes start digesting the pancreas and surrounding tissues, leading to chronic pancreatitis.
Symptoms of Chronic Pancreatitis
Chronic pancreatitis exhibits the following symptoms:
- Severe recurrent pain in the upper abdominal
- Diabetes mellitus due to insulin underproduction
- Malnutrition, diarrhea and weight loss
Chronic pancreatitis can further lead to bleeding within the abdomen, abscess formation and also increase your risk of developing pancreatic cancer.
Diagnosis of Chronic Pancreatitis
To diagnose chronic pancreatitis, your doctor may perform a physical exam where your abdomen will be palpated to check for a lump. Your doctor may also order certain tests to confirm the diagnosis including blood tests, ultrasound, CT and MRI scans, endoscopy, endoscopic retrograde cholangiopancreatography (ERCP) and biopsy of the pancreas.
Untreated Chronic Pancreatitis
Left untreated, chronic pancreatitis worsens causing permanent damage to the pancreatic tissues.<
Treatment for Chronic Pancreatitis
- Treatment depends on the severity of chronic pancreatitis.
- You will be advised to abstain from smoking and excessive intake of alcohol.
- You will be prescribed pain medication.
- Treatment will be focused on your nutrition. You may require hospitalization for intravenous hydration and nutritional support. In cases of continued weight loss, you may be fed through a tube inserted into your nose, that runs down your throat and into your stomach (nasogastric feeding).
- Synthetic pancreatic enzymes may be prescribed if your pancreas does not produce enough, once you return to your normal diet.
- You will be prescribed insulin if your pancreas does not produce enough insulin.
- Surgery may be required if there is a block in the pancreatic ducts.
Indications for Surgery
Surgery is usually considered to remove any blockages in the pancreatic ducts. Common indications for surgery include:
- Recurrent upper abdominal pain
- Pancreatic Tumor
- Infection or cysts in the pancreas
- Obstruction in the bile duct or duodenum (small intestine)
- Pancreatic ascites or fistulae
Surgical Procedure for Chronic Pancreatitis
Surgical procedures for the treatment of chronic pancreatitis are usually performed under general anesthesia with you lying on your back. These may include:
Drainage procedures: This procedure is performed to release the excess pressure in the pancreatic ducts caused by an obstruction, and relieve pain.
A small incision is made in the abdomen to access the pancreas. The pancreatic duct is opened up along the length of the pancreas and drained. Any stones present in the pancreas are also removed. A Roux-en-Y jejunostomy is then performed to reconstruct the gastrointestinal tract, where the pancreas is sutured to the jejunum (section of the small intestine). The incision is closed with stitches. Examples include Duval’s, Puestow–Gillesby and Partington–Rochelle procedures.
Resection procedures: These involve the surgical removal of the head of the pancreas. Examples include Kausch–Whipple pancreaticoduodenectomy (PD), Pylorus-preserving pancreaticoduodenectomy (ppPD) and Beger operation (duodenum-preserving pancreatic head resection [DPPHR]).
Resection and drainage procedures: These involve drainage as well as the removal of a part of the pancreas. Examples include Frey procedure and Izbicki procedure.
Pancreatectomy: This procedure involves partial or complete removal of the pancreas. In cases of complete removal, the pancreas is replaced with functional cells that aid digestion which is extracted from the healthy pancreas and infused into your liver.
Risk and Complications
Surgery for chronic pancreatitis may have certain risks and complications such as:
- Infection
- Pain or swelling at the incision site
- Injury to nearby tissues

